Alliance RetinaIt's Simple-All Patients, All Problems, All the Time
-
Diabetic Retinopathy
About Diabetes Diabetes is one of the leading causes of visual loss in the United States. Visual problems become more likely the longer that diabetes has been present. Given enough time, about 85% of diabetics will have some eye problems. Over many years, good blood sugar control does limit, but does not prevent, eye problems.
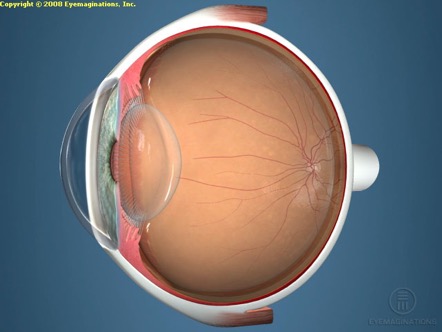
Diabetes affects the eye in two main ways. First, excess sugar can be trapped in the eye’s lens causing blurry vision, a change in glasses prescription, and cataracts (cloudy lens). Diabetics frequently require more changes in their glasses prescription and need earlier cataract surgery than the average patient. Second, diabetes causes the smallest blood vessels in the back of the eye to close down or leak. Damage here, in the retina, causes the most severe threat to vision.
What is Diabetic Retinopathy?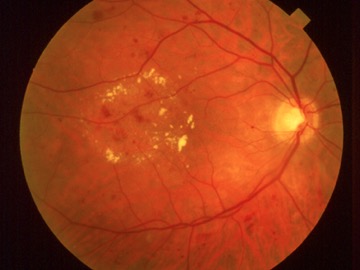
The eye is like a tiny camera, and the retina is the “film” in the back of this camera. The center of the retina is a tiny spot called the “macula”, which supplies all of our sharp, central vision. The earliest form of diabetic retinal damage is called “background diabetic retinopathy”. About 50% of patients with diabetes for 10-15 years have some signs of this such as bleeding, or swollen pockets within the retina. If these swollen areas affect the macula, dim or blurry vision may result.

If the eye disease worsens, areas of the retina may not get enough blood. The eye responds by growing thin new vessels. This is called “proliferative diabetic retinopathy”. Unfortunately, these new vessels frequently break open and bleed, filling the eye with blood and stimulating scar tissue to grow, sometimes leading to retinal detachment. The early stages of this condition can be treated with the laser. More advanced disease often requires invasive surgery, called “vitrectomy”, which involves removal of blood, scar tissue, and abnormal vessels within the eye and repair of retinal detachment.
How is Diabetic Retinopathy detected?
In some cases, advanced damage may be present without the patient even being aware. Also, most treatments for diabetic eye disease work better at preventing and controlling the diabetic retinopathy than at reversing it once it is well established. Because of this, it is very important for diabetics to have a regular, complete eye examination that should include drops to dilate the pupil. We recommend regular eye examinations, in most cases once a year, to detect diabetic eye problems before the patient recognizes visual problems. We routinely report information about your exam to your primary care physician and/or diabetes specialist to keep them updated on this part of your health. In between scheduled eye examinations, patients should report any changes in their vision, such as increased fuzziness, new floating spots, restricted side vision, or pain.
In addition to regular eye examinations, the diabetic patient should work with his or her physicians to control the blood sugar level and keep blood pressure under control. Tests to determine how well the kidneys are working may also be needed. Over years, this has been shown to reduce the severity of diabetic complications. Diabetic patients who become pregnant should have even more frequent examinations of the retina.
How is Diabetic Retinopathy treated? When significant retinopathy is detected, a special test called fluorescein angiography is sometimes performed. This is a photographic test of the retina and does not involve X-rays. After color pictures are taken, a yellow dye
called fluorescein is injected into the arm vein and photographed as it passes through the retinal vessels. This provides a very detailed "road map" of the retina, identifying any weakened or abnormal blood vessels. This test is helpful in deciding whether laser treatment is needed and in guiding that treatment.
Laser surgery is the most common treatment for diabetic retinopathy. Laser is a highly focused beam of light that can be used to cauterize leaky blood vessels or stimulate abnormal new vessels to shrink and stop bleeding. Laser surgery is done in the office, using anesthetic eye drops or an anesthetic injection. Usually laser involves little or no discomfort, and patients go home immediately after treatment. Post-operative discomfort, if it occurs, is usually controlled with non-prescription pain medication such as Tylenol TM or Advil TM.
Laser surgery for retinal swelling is called focal or grid laser therapy. This is effective in preventing further vision loss and may result in some visual improvement. Once this treatment has been performed, it may take several weeks or months for the swelling to fully drain away. Occasionally, more leaky spots develop requiring repeated focal treatment. Abnormal new vessel growth can be treated with panretinal photocoagulation. In this type of laser surgery, a large number of laser spots are placed in the side portions of the retina. This causes abnormal new vessels to shrink and reduces the risk of vision loss from bleeding or retinal detachment.
Laser surgery is designed to stabilize or improve vision. It cuts in half the risk of severe vision loss. Even if vision is not improved, laser therapy may help to limit visual loss that would have occurred without treatment. Some patients experience side effects of laser, including m ild loss of side vision, blurry vision or spots in the vision, difficulty seeing in dim light, or sensitivity to light. These side effects, when noticed at all, are usually mild and temporary, but on occasion they may persist. Even then, this is far better than the serious visual loss that can result without laser treatment.
Although laser treatment is very successful at stabilizing diabetic retinopathy, it is not a cure. Sometimes, damage may progress despite laser treatment. This damage can include persisting hemorrhage in the central jelly, called Vitreous Hemorrhage (shown at right), or scar tissue and detachment of the retina. Vitrectomy surgery may be needed if further hemorrhage or damage to the retina occurs in spite of laser or if laser has not been performed before these more serious problems occur. This is an operation in which the jelly in the back of the eye along with any scar tissue or blood is removed. This is usually a very successful procedure that is well tolerated by the eye. Your doctor can discuss your case with you individually.
-
Macular Degeneration
Why Is the Macula Important? Unlike a photograph in which the entire picture is in focus, our eyes can only focus on the object at which we are looking directly. (Try reading the first word of this sentence while staring at the period at the end of the sentence).
The macula is responsible for our clear central vision. The remainder of the retina is used for side or peripheral vision. Damage to the macula causes blurring of our central vision which may make it difficult to read, drive, watch television, and recognize familiar faces.
What is Age-Related Macular Degeneration? Macular degeneration is the leading cause of poor vision in the United States. Each year, approximately 170,000 new cases of age-related macular degeneration (AMD) are discovered. Macular degeneration occurs whenever a previously normal macula begins to deteriorate. Juvenile macular degeneration begins at a young age and is quite rare. AMD is very common and occurs in older people, although getting older does not always result in visual problems.
As AMD progresses, the central vision begins to blur, but the peripheral vision remains normal. Please remember that macular degeneration does not cause total blindness. Even at its worst, AMD spares peripheral vision and allows patients to care for themselves. Macular degeneration often affects both eyes, although the second eye may not become involved for many years.
There are two main types of AMD, dry macular degeneration and wet macular degeneration.
Ninety percent of macular degeneration patients have the dry form. The cells in the macula slowly wear out. The loss of central vision is often mild. Some patients may have progressive deterioration, usually over a long period of time, resulting in severe loss of central vision. Only 10 percent of severe loss of central vision is due to dry AMD.
The more severe wet (exudative form) affects 10 percent of macular degeneration patients. In this type, fluid may collect or abnormal blood vessels may grow underneath the retina. They often cause severe damage to the vision from bleeding and scarring under the macula. The wet form accounts for 90 percent of the patients with severe loss of central vision.
What Causes Age-Related Macular Degeneration? Aside from aging, no specific cause of macular degeneration has been identified. Heredity plays a role in many patients. The disorder is limited to the eye and is not associated with problems elsewhere in the body. Tumors and infections are not associated with macular degeneration. Extensive use of the eyes, reading or watching television does not cause macular degeneration or result in further damage. There is nothing a person can do that will accelerate or retard the progress of AMD.
How Do I Know if I Have Macular Degeneration?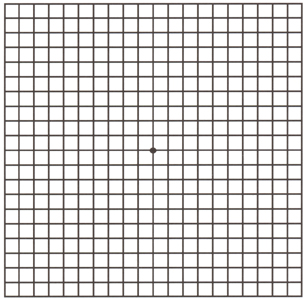
Most people with macular degeneration have either blurred or distorted vision in one or both eyes. Distorted or wavy vision is a very important symptom and should be reported promptly to your doctor. This is especially true when straight lines (doorways, telephone poles, etc.) appear wavy. Many people with visual loss in one eye may not realize they have a problem because the good eye takes over for both eyes.
You will be given a special Amsler grid test to be used at home to help you recognize early changes in your vision or identify new areas of distortion This grid test should be used on a daily basis. It is very important to check each eye separately. There is a sample grid at the end of this booklet with instructions for its use.
What Tests Can I Expect? The doctor will examine your eyes on each visit. If necessary, he may order a fluorescein angiogram. In this test, a dye is injected into an arm vein, and pictures are taken of the macula as the dye circulates through the blood vessels. In some cases, another type of angiogram, called High Speed-ICG, is used to take a movie of the deepest layers of the eye using a different dye and a special infrared camera.
Because the vessels of the eye can be photographed directly, no X-rays are involved and the tests are safe for patients who are allergic to X-ray dyes. Patients allergic to Iodine should only have High Speed-ICG with special precautions. The angiogram provides a detailed picture of the retinal blood vessels and will detect any abnormal vessels that might be present. The doctor uses this information to determine whether treatment might be helpful. The dye is excreted in your urine for up to 24 hours following the injection. The whites of your eyes and your skin might turn slightly yellow for a day. Hospitalization is not required for this test, and you are free to go home when it is finished.
Another very common test is Optical Coherence Tomography, or OCT. This is a simple and painless snapshot that takes extremely detailed images of the macula.
What Treatment Is Available for Macular Degeneration?
There are no eye drops or operating room surgeries that have been shown to be effective in curing macular degeneration. The current standard of care for "wet" macular degeneration is clearly treatment with Vascular Endothelial Growth Factor (VEGF) inhibitors, particularly Avastin, which is preferred by a significant majority of retinal doctors around the world. Conventional laser treatment only benefits a small percentage of macular degeneration patients who have certain types of the wet form. However, laser can stabilize vision and prevent further deterioration and in some cases, improve vision to some degree.
Conventional Laser Treatment
Conventional laser consists of a strong beam of light, which enables the physician to seal (cauterize) the abnormal blood vessels, which may grow in the wet form of macular degeneration. Before the laser procedure, an anesthetic injection may be used. The injection often causes the vision in the treated eye to be blurred for several hours. You will be in a sitting position for the treatment. The actual laser treatment, which is not painful, usually takes less than 5 minutes. You will be able to return home immediately and resume your normal activities within 24 hours. Unfortunately, only some types of wet AMD respond to conventional laser. Laser treatment does not cure macular degeneration, and it does not necessarily prevent abnormal blood vessels from returning in the future. It is important for you to continue to test your vision with the Amsler grid chart. If further changes are noted, they should be reported promptly to your doctor. If the abnormal blood vessels do return, it may be possible to treat them with laser again. Outmoded Laser Techniques Abnormal new blood vessels may grow into the very center of the macula in some cases of macular degeneration. These vessels may grow in a variety of patterns. Depending on the pattern of leakage, one previous technique was photodynamic therapy. This involves injection of a medicine called Visudyne, which is selectively absorbed by abnormal, growing blood vessels. The medicine is allowed to adsorb for 15 minutes after beginning infusion through an intravenous line. Red laser light is then shown into the eye, which activates the medicine. This chemically cauterizes the abnormal blood vessels as well as the surrounding normal tissue. This results in visual improvement in only about 15 to 20 percent of cases, but prevents further vision loss in another 50 to 60 percent. A significant percentage of patients are actually made worse by the procedure, and it is very difficult to predict who may be harmed. In some cases, transpupillary thermal therapy, another older treatment technique has been used. Instead of applying a hot laser, which burns the tissue that it touches, transpupillary thermal therapy involves gently heating this area with much cooler laser settings. This results in very mild photocoagulation of the abnormal tissue, with less damage to surrounding normal tissue. This has been shown to stabilize or improve vision in 50 to 70 percent of patients with this pattern of leakage. All of these treatments seek to treat the area of leakage directly. These leaky blood vessels grow in a pattern like a small flat tree or bush underneath the retina. In some cases, it would be just as effective to treat the underlying trunk blood vessel, which feeds this tree. In the past, available cameras have not been able to visualize the feeder vessel. Using a more advanced camera we can, in many cases, visualize this feeder vessel. Feeder vessel therapy has been shown to be useful in some cases not treatable by other means.
Vascular Endothelial Growth Factor (VEGF) Inhibitors
Avastin- Although all of these laser techniques are of historical interest, they are no longer widely used, if used at all. The current stand of care is clearly treatment with Vascular Endothelial Growth Factor Inhibitors. Avastin is an FDA approved medication that inhibits the growth of new blood vessels. It was originally approved for the treatment of colorectal cancer, but it has been shown to be effective with macular degeneration as well. The data on Avastin shows that it is clearly and vastly superior to Macugen or most other treatments, resulting in actual visual improvement in many patients far more often than other treatments. It is an antibody which inhibits abnormal vessel growth by binding and inhibiting a substance called Vascular Endothelial Growth Factor, or "VEGF". This substance is abnormally present in eyes with certain conditions that cause abnormal vessels to grow and bleed within the eye. Avastin, when injected into the eye, can inhibit this process and reduce leakage and bleeding, hopefully stabilizing or even improving vision. Prior to injection, the eye is sterilized and anesthetized, and the injection is general very safe and not unpleasant for the patient. The major risks, each individually rare, are infection, bleeding, cataract, or retinal detachment. For this reason, we watch the eye very closely after injection and recheck the eye, generally within 1 to 2 weeks after injection. There is a report of higher risk of blood clots leading to problems such as heart attack or stroke after using IV Avastin in cancer patients in high doses (up to 1500 mg. IV) combined with 5-Fluorouracil, another cancer drug, intravenously every 2 weeks. This was only found in colon cancer patients. By comparison, we use 1 to 2.5 mg. injected into the isolated space of the eye every 2 or 3 months. Genentech, the company that makes Avastin, advised at the time of that report not to apply this precaution to clinical situations other than colon cancer patients receiving this high dose Avastin in combination with 5-Fluorouracil. We are none-the-less mindful about this and only recommend Avastin when we believe the benefits clearly outweigh the risks. When used alone, Avastin intraocular injections have been found to have a very high safety profile. Avastin injection may need to be repeated every 1 to 3 months for several injections. With concurrent use of various laser techniques, it may not be necessary to repeat injections as often. There is some evidence that giving a dose every month for three doses and then cutting back to reinjection only as needed may have a better visual result in some people. We will watch your progress very carefully during this type of therapy and discuss your individual circumstances with you.
Lucentis- Another drug, Lucentis, is actually a slightly altered fragment of Avastin, which has fewer active sites. It may work as well as Avastin, but many doctors do not believe it works for as long. It is thousands of dollars more expensive and can result in considerable cost to the patient. There is considerable controversy surrounding Lucentis and why it was really developed in the first place. Because of this and the likely therapeutic superiority of Avastin, we recommend Avastin in most cases where an injection is recommended.
Macugen was the first FDA approved medication that inhibits the growth of new blood vessels, and at this time is really only of historical interest. In practical experience, Macugen rarely improves vision. Vision loss is often slowed, but, as with Photodynamic Therapy, most patients do continue to lose vision. There are no compelling medical reasons to use Macugen or to switch from Avastin to Macugen in ongoing therapy.
Systemic Medications
No systemic medications have been proven to be effective for macular degeneration, except for intravenous Avastin, which is safer and more effective given as an intraocular injection. Some research, however, suggests that certain dietary supplements may help. Vitamins and minerals such as zinc, vitamin E and selenium are advocated by some researchers for the purpose of trying to prevent further visual loss from dry macular degeneration. Other substances that have received much attention include Bilberry and Lutein. Current studies may determine whether these medications are really helpful. Your doctor will discuss them with you if he or she feels they might be appropriate for you. Dietary Measures
In addition to the vitamins listed above, some people do believe that certain foods, which contain these vitamins, or other factors may help control the progression of macular degeneration. Such foods include dark green leafy vegetables, red wine (particularly the Cabernet, Pinot Noir, and Syrah grapes) and other foods rich in antioxidant vitamins.
Surgery
Very few patients with AMD will need surgery. Surgery may be considered when abnormal new vessels grow in the center of the macula or when a very large hemorrhage occurs. These are instances in which the eye is threatened with severe visual loss. Your doctor will discuss this further if it is appropriate.
New Research
There are many new research studies under way to look for other treatments for specific types of macular degeneration. We will keep you posted on new developments as news becomes available. Unfortunately, in recent years there has been a growing practice of disguising marketing efforts as "research", where doctors are paid by drug companies to recruit patients for exercises to expand markets for the most expensive drugs regardless of whether this is in the patient's best interest. We have been active on a national level advocating for patients' rights, and particularly to illuminate relationships with industry where doctors have a financial interest in using patients in this way. We work very hard to separate real research from such practices, and we will try to keep you informed about legitimate new findings.
Low Vision Aids
For those patients with AMD who lose central vision, low vision aids may help to maintain the ability to do everyday tasks. These aids range from spectacle and hand-held magnifying glasses to special lighting devices. Telescopic clip-on lenses to fit over your present glasses are sometimes
used to improve distance vision. Special television systems may help restore slow reading ability to those patients who have severe loss of central vision. Low vision aids are prescribed by specialists who will be recommended by your doctor if
appropriate. The Sight Center of Toledo provides these services and works very closely with Vision Associates, seeing patients at the Vision Associates offices every Tuesday.
In addition, the New York Times prints a weekly newspaper in large print for those with limited vision. (The New York Times Large Type Weekly, P.O. Box 2570, Boulder, Colorado 80303); Reader's Digest also publishes in large print. (Reader's Digest Association, Pleasantville, New York 10571); Large print books are published by G.K. Hall, (70 Lincoln Street, Boston, Massachusetts, 1-800-343-2806) and are available at most book stores.
It is encouraging to know macular degeneration does not lead to total blindness, but only to the loss of the central portion of the vision. Side vision is retained in all cases. Low vision aids, rarely restore normal reading vision, but may offer significant help. Click Here for information in a simple overview lecture.
What to do if you have Macular DegenerationHave a regular eye examination at least once yearly. If you are seeing a retinal specialist as well as your general eye doctor, you may be able to alternate visits to maximize convenience and reduce cost.
Use an Amsler grid at home to monitor your vision. Look at the chart from reading distance using any bifocals or reading glasses you normally use. All you have to do is take a quick glance. If you stare at it for too long, the image will fluctuate and become confusing.
Quit smoking and control your blood pressure at well as you can. Both of these measures may help.
At least consider using antioxidant vitamin supplements. There is some evidence that these may help stabilize the wear and tear process. There are three reasonable options:
Use a multivitamin such as Centrum Silver or an equivalent,
Use an “eye vitamin” such as Ocuvite or I-caps. As a rule of thumb, you should not have to spend more than about $15.00 a month on this. If you are spending more, you may be using something that is less proven or be a victim of a marketing scam.
Go “ala carte” using single preparations including Vitamin A, D, E, C, B complex, zinc, and selenium. Other supplements that may help include Lutein, zeaxanthine, Billberry, and Ginko biloba. If you are a smoker, you should avoid Vitamin A, as this may increase the risk of lung cancer. You may use Lutein, which is a similar "carotene" molecule.
The most convenient choice is to use an eye vitamin, which contains Lutein either with or without a multivitamin. It is also reasonable for your younger family members to consider using these, since the disease has a hereditary component, and the vitamins may have a preventative effect.
Eat well and consider including food types that are suggested to have beneficial effects. These would include dark, green leafy vegetables such as spinach, other sources of the vitamins listed above, and red wine (especially from the Cabernet and Syrah grapes).
-
Ocular Histoplasmosis
What is Histoplasmosis? Histoplasmosis is a disease caused by a fungal organism, which is commonly found in the soil mostly in the Midwestern United States. There are two basic types of histoplasmosis, systemic and ocular. Systemic histoplasmosis produces an influenza-like illness with fever and weakness that usually lasts about two weeks. After recovery, the infection can leave small, usually harmless, scars throughout the body. The eye can be involved and the scars can be detected during an examination of the retina. Visual problems never develop during the initial, acute infection.
What Is Ocular Histoplasmosis? Most people with healed “histo” scars in the eye do not develop further problems. However, abnorma
l blood vessels may begin to grow through the healed histoplasmosis scars many years later. These abnormal blood vessels may cause bleeding and further scarring which can damage the retina. If the abnormal blood vessels are near the central part of the retina (the macula), reading vision may be damaged. Early diagnosis and treatment of these abnormal blood vessels is very important. Visual problems from ocular histo can occur long after the systemic phase.
How Will I Know if I Am Developing Ocular Histoplasmosis?
Most people with active ocular histoplasmosis have blurred or distorted vision in one or both eyes. Distorted vision is a very important symptom and should be reported promptly to your doctor. This may appear as straight lines looking wavy (doorways, telephone poles, flagpoles, etc.). Many people with decreased vision in one eye may not realize they have a problem because the remaining good eye compensates so well. It is very important to check each eye separately. Ocular histoplasmosis may affect both eyes, although the second eye may not become involved for many years.
Ocular histoplasmosis is diagnosed with an eye examination involving dilation of the pupils. A special photograph test, which is often helpful, is fluorescein angiography. In this test, dye is injected through an arm vein and pictures are taken of the eye as the dye circulates through the retina. These pictures are helpful in diagnosis and also serve as a road map for possible laser treatment.
What Treatment Is Available for Ocular Histoplasmosis? There are no eye drops or antibiotics known to be effective in ocular histoplasmosis. When abnormal vessels grow outside of the centermost part of the macula, laser surgery has the best chance of stopping the progression of abnormal blood vessels. If the vessels are growing in the very center, newer laser techniques may help. Sometimes it is possible to do a delicate operation to reach under the retina and physically remove them.
What Is Laser Treatment Like? Laser is a precisely focused beam of light, which can seal (cauterize) tissue in the
retina. The laser beam seals abnormal vessels but does not help already damaged retinal tissue to function better. If some of the visual decrease is due to swelling from leaky blood vessels rather than scar tissue per se, then laser may actually help vision by allowing the swelling to subside. Laser surgery is done in the office and is not painful. After the treatment, you will be free to return home. Unfortunately, laser surgery does not always eliminate abnormal blood vessels. In some cases, additional treatment may be needed. Even if vision is not improved, laser therapy may help to limit visual loss and minimize damage that would have occurred without treatment.
Can I Prevent Ocular Histoplasmosis? The factors that cause active histo are poorly understood at this time. The body's immune system may play a role. No special diet or medical treatment has been shown to prevent the formation of abnormal blood vessels. If you have macular histo scars, you should monitor your vision at home with an “Amsler Grid”, or a piece of graph paper and report any sign of distortion or decreased vision to your doctor promptly. Remember, the earlier the diagnosis is made, the better the chance of saving the reading vision. Laser treatment for histo scars that are not active has not been shown to be effective.-
Cystoid Macular Edema
What Is Cystoid Macular Edema? The healthy retina is a very thin tissue, which lines the back of the eye. The retina functions as the film in the back of the camera. The central portion of the retina is called the macula. This area provides all of the sharp central vision
for activities such as reading and driving. This area is very delicate and can develop swelling, or “edema”, when it is irritated. This swelling makes the macula look bubbly or “cystic”, hence the name cystoid macular edema, or “CME”.
Who Gets Cystoid Macular Edema? Cystoid macular edema can occur in different conditions and is seen occasionally in patients who have had previous eye surgery. Only a small percentage of people who have had cataract or other eye surgery will develop cystoid macular edema. The swelling may occur many months or even years after the surgery. It can occur with all types of cataract surgery and with any type of lens implant. Cystoid macular edema may occur despite perfect surgery without any complications.
CME may also occur as a result of inflammation inside the eye, or from weak blood vessels as in diabetes or with blocked retinal veins. Inflammation can result from infection, autoimmune inflammation (called “uveitis”), trauma, or other irritating stimuli. Cystoid macular edema may occasionally develop for no apparent reason.
What Are the Symptoms of Cystoid Macular Edema? Patients with cystoid macular edema frequently notice their reading vision is blurred. The peripheral or side vision remains unchanged. Frequently, people with cystoid edema notice distortion of objects and dimness. In addition, eyes may appear irritated and red, may water a great deal, and may even be tender to the touch.
How is Cystoid Macular Edema diagnosed? If cystoid edema is suspected, a picture test called a fluorescein angiogram may be performed. During the test, color photographs of the retina are taken, after which a yellow dye is injected into an arm vein. Photographs of the retina following dye injection indicate pooling of dye in the macula in a distinctive pattern, confirming the diagnosis of cystoid macular edema. Sometimes, the cystoid edema can be seen without the need for angiography.
What Treatments Are Available for Cystoid Macular Edema? Depending on the severity and the cause, cystoid macular edema may be treated in a number of ways. If the swelling has resulted from an observable problem, such as an infection, then treating the cause may help. Edema from diabetes is often treated with laser to seal leaky diabetic vessels. If a problem related to previous surgery is detected, such as a piece of leftover retained cataract, additional surgery may be performed to resolve this issue.
Usually, initial treatment for simple postoperative macular edema consists of using anti-inflammatory eyedrops, sometimes along with an over-the-counter anti-inflammatory pill, such as Aleve TM. If this is not adequate, anti-inflammatory steroid injections may be placed around the eye, or given in high doses intravenously. In rare cases, the vitreous jelly, in the back of the eye, may be removed in an attempt to decrease irritation or tugging on the back of the retina. If the edema is felt to be due to irritation from a lens implant, that implant may need to be surgically removed or exchanged for another style of implant.
Steroid medications can sometimes cause abnormal elevation of pressure in the eye, requiring additional medications to control this pressure. For this reason, use of these medications must be watched closely. Cystoid macular edema usually responds well to treatment, although response may require several months of continuing treatment. In rare cases, cystoid macular edema, and vision loss, persists in spite of all treatment attempts. Your doctor will discuss your individual case with you.-
Macular Cellophane (Pucker)
What is a macular pucker? The eye is like a tiny camera, with lenses in front and film in the back. The film in the back of
the eye is called the retina. The center part of the retina, which provides most of the reading and other sharp, central vision is called the macula. The area in front of the retina is normally filled with a jelly-like material called vitreous. At birth, the vitreous is quite firm and has thin fibrous strands running through it and a clear fibrous skin on the back. As the vitreous ages, it becomes more liquid. Eventually, the fibrous skin peels partially or totally away from the retina. This process, called vitreous detachment, increases the number of floaters but does not usually cause damage to the retina. Occasionally the vitreous can cause irritation to the macula, which can stimulates the formation of a thin sheet of scar tissue on the macular surface. This looks like cellophane and is sometimes called “cellophane maculopathy”. The scar tissue may thicken or contract over a period of time. This can distort or “pucker” the macula, causing significant visual distortion. This condition is called a macular pucker.
How is Macular Pucker diagnosed?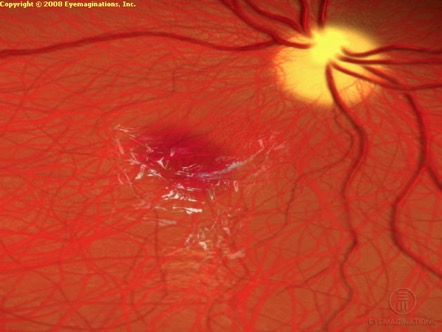
Macular pucker causes fairly typical symptoms, although these symptoms are sometimes confused with macular degeneration, which is a totally different condition. It has a very typical appearance and is usually easy to diagnose with a dilated eye examination. Sometimes a special computerized picture test called a fluorescein angiography is performed to rule out other problems under the scar tissue, and to find inflammation sometimes associated with the pucker. This involves injection of a yellow dye into a small arm vein, which is then photographed as it flows through the circulation in the back of the eye. There are no X-rays, and the dye is generally very safe, with serious allergic complications being very unusual.
How is Macular Pucker treated? If the visual change is minor, and the patient is still able to function comfortably, then no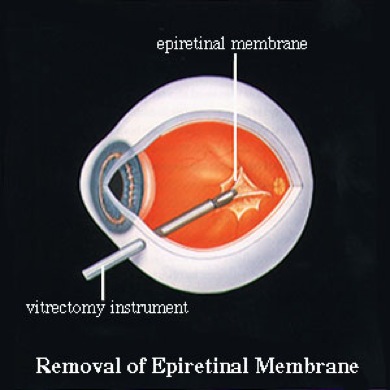
intervention may be necessary. If the pucker is severe enough to prevent the patient from seeing and doing what they would like to, then the scar tissue can be surgically removed. This involves an operation called a vitrectomy. Tiny needle-sized openings are made in the white part of the eye. Tiny instruments, the size of hypodermic needles, are then used to gently peel the scar tissue away from the macular surface. The vitreous gel is removed to gain access to the macula. It is replaced with a clear fluid that the eye naturally replenishes continuously.
Vitrectomy surgery is usually done as an outpatient. The experience for the patient is similar to having cataract surgery. There may be some scratchy feeling on the day after surgery, but typically there is no severe pain. This surgery is usually done with a local anesthetic injection behind the eye. Complications, such as bleeding, infection, and retinal detachment are very unusual.
Visual recovery may take weeks to months, but the eye will feel relatively comfortable within days of the surgery. The patient can usually resume normal activities within one or two weeks after surgery. Your doctor will discuss your individual case with you.-
Macular Hole
What is a Macular Hole? The healthy retina is a very thin tissue, which lines the back of the eye. The retina functions like the film in the back of a camera. The central portion of the retina is called the macula. This area provides all of the sharp central vision for activities such as reading and driving. If this area is damaged, the central vision can be severely affected. A macular hole, as the name implies, is a condition that causes a hole to develop in this central area. Macular holes may occur in a number of ways. They may occur after trauma to the eye or from inflammation in the eye. Holes forming from these conditions are more difficult to treat and have a lower chance of visual improvement. The most common cause of macular hole formation is simple traction, or tugging, of the vitreous gel on the macula. The vitreous is a bag of gel that fills the back of the eye and presses against the retina. With age, the gel can become watery in its center and the skin on the back can tighten and become thicker, pulling on the macula. This can stretch the macula until it breaks at its center. This results in progressive loss of the central but does not usually affect the peripheral vision. The vision usually decreases to the “E” at the top of the eye chart but usually not further.
What Are the Symptoms of Macular Holes? Patients who develop macular holes initially notice distortion and waviness in the central vision, especially while reading. This may slowly or abruptly worsen. In some cases, the other eye compensates well enough that the patient notices no vision loss until they cover the good eye. The peripheral or side vision remains unchanged.
How are Macular Holes Diagnosed?
Macular holes can be diagnosed with a full eye examination, including drops to dilate the pupil. Optical Coherence Tomography, or OCT, is new type of imaging that can very precisely diagnose macular holes, even in their very early stages. Sometimes it is necessary to look for associated macular swelling with a photographic test called fluorescein angiography. During the test, photographs of the retina are taken and a yellow dye is injected into an arm vein. Photographs of the retina following dye injection may show pooling of dye in the macula in a distinctive pattern, confirming the presence of swelling associated with the hole.
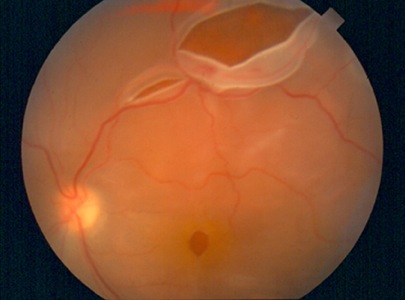
What treatments are available for macular holes? Macular holes resulting from vitreous traction can be closed with an operation called vitrectomy. In this procedure, the eye is anesthetized and the vitreous gel is then vacuumed out and replaced with fluid. If there is any thickened gel, it is peeled from the macula. The eye is then filled with a gas mixture. The surface of the gas bubble presses against the macula closing the hole. The surgery is usually done as an outpatient and is not painful afterwards. You will use eyedrops for a couple of weeks after the surgery.
In order for surgery to be effective, the bubble must press directly on the macula, which is at the very back of the eye. It is therefore critically important that the patient look straight down continuously for two weeks. This is by far the most important factor for success. Patients may utilize special chairs, beds, and other equipment to make this easier. Your doctor can discuss this further with you.
As an alternative, the eye can be filled with liquid silicone oil. This, like the gas bubble has a 90% success rate, but the silicone must be removed after about 3 months, so this does require an additional procedure.
This surgery, and especially the gas bubble, may result in more rapid cataract formation than normal. This is treatable with routine cataract surgery. In some cases, cataract surgery is combined with vitrectomy surgery for macular holes. Your doctor will more fully discuss these issues with you, and answer any questions you may have.
Surgery succeeds in closing the hole in 80-90% of cases. In 60-70% of cases, this results in vision improvement. If there is too much “wear and tear” from having had the hole, vision may not improve. Complications are very unusual but include bleeding, infection, and retinal detachment. Your doctor will discuss this with you and watch very closely for problems in the postoperative period.-
Retinal Vein Occlusion
The eye is like a tiny camera, with lenses in the front and film in the back. The “film” in the camera is called the retina. It is nourished by tiny blood vessels. Arteries carry the blood into the back of the eye, and veins drain the blood out and back to the heart. Sometimes, the main vein that drains blood from the eye can become blocked. This is called a central retinal vein occlusion (CRVO), and can result in mild to severe vision loss.
If this process occurs in one of the small venous branches, it is called a branch retinal vein occlusion (BRVO). Similar loss of vision can occur, but it is usually more localized and less severe. In the picture at right, the central vision is decreased because the blockage is very near the macula, which provides reading vision. If the macula is not affected, there may be little or no vision loss at all.
When a vein occlusion occurs, the vision may be damaged in three main ways. Blood may back up and break out of blood vessels resulting in hemorrhages that block the vision. Fluid in the bloodstream may leak out of vessels resulting in vision loss from swelling, also called “edema”. Finally, the capillaries (the tiniest vessels) may be damaged, decreasing oxygen supply to the retina enough to result in vision loss. The macula is the central portion of the retina responsible for sharp central vision. If the macula is involved in the occlusion, vision loss may result.
What Causes Venous Occlusion?
Vein occlusions may have many causes. In elderly patients, they are more common in patients with other diseases of small blood vessels such as diabetes and high blood pressure. Patients of any age may have blood disorders that result in abnormally thick blood causing vein occlusions. If you have not had a recent medical exam, you should have one to check for these possible associated conditions. Glaucoma, a condition involving increased eye pressure, may cause vein occlusions by increasing resistance to blood flow within the eye. We will check for this as part of your evaluation.
How Is Venous Occlusion Diagnosed?
Vein occlusions can be detected by examining the back of the eye after instilling drops to dilate the pupils. Sometimes, the circulation is more closely studied using a picture test called fluorescein angiography. This involves injecting a synthetic dye, called sodium fluorescein into an arm vein. A few seconds after injection, this dye appears in the retinal vessels and is photographed with a special computerized camera, providing a very detailed “roadmap” of the circulation.
What treatments are available for venous occlusion?
The treatment of retinal venous occlusion depends on the size and location of the blocked vessel. Some small vein occlusions are self-limited and resolve on their own without the need for treatment. The hemorrhage from vein occlusions clears with time and does not require treatment. The swelling that often results from vein occlusion may persist for long periods. In many of these cases, laser treatment can be used to seal leaky vessels and assist in the reabsorption of this swelling. One complication of vein occlusion is abnormal new vessel formation in the eye that can result in vitreous hemorrhage with sudden vision loss or a severe, painful form of glaucoma. These complications can be treated with other laser techniques. Some severe vein occlusions have been successfully treated by doing surgery to physically relieve the site of blockage. Your doctor can discuss with you what, if any, treatment is recommended in your case. While vision cannot always be restored in eyes with vein occlusions, in many cases the vision can be stabilized or restored.-
Retinal Artery Occlusion
What is the carotid artery? The two carotid arteries are the main arteries in the neck. They supply blood to the head, including the eyes and the brain. One carotid artery supplies the right side, while the other serves the left. Cholesterol and blood clots can form in the carotid artery, which can cause blockage at that site or can break off in small pieces that flow downstream and cause blockage of smaller branches in the eye or brain. Because the eye and the brain share the same source of blood supply, blockages or conditions of the carotid artery can affect either.
What happens when the carotid artery is blocked? Depending on where the blockage occurs and how complete the blockage is, different symptoms can result: If a piece of cholesterol or a blood clot breaks off from the carotid artery and travels to the eye, the circulation to some part or all of the retina can become affected. A Central Retinal Artery Occlusion (CRAO) occurs when the main artery to the retina becomes totally blocked, causing sudden total vision loss. Later complications may include growth of abnormal vessels and bleeding inside the eye, or a severe, painful form of acute glaucoma (high eye pressure). In a Branch Retinal Artery Occlusion (BRAO), one of the smaller branches inside the eye is blocked, and only a portion of the vision may be lost. This appears as a sudden “blackout” of a segment of the vision. Sometimes, a piece of cholesterol, known as a Hollenhorst Plaque, can be seen at the edge of the blockage, such as in the picture at right. Sometimes such a plaque is seen in a retinal artery with no sign of active blockage. Although this causes no symptoms, it serves as a warning sign of possible imminent problems. When the branches of the carotid artery going to the brain are blocked, a Cerebrovascular Accident (CVA or stroke) may result. Depending on the part of the brain involved and the size of the area affected, the effects of a stroke may be mild or devastating. Severe effects can include paralysis of one side of the body and loss of speech. If the part of the brain having to do with vision is involved, a stroke can lead to loss of side vision. If blood supply to the eye or brain is slowly cut off, more subtle symptoms may occur. Chronic poor circulation to the brain can cause dementia-like symptoms and vague neurologic problems. Slow circulation to the eye, known as Ocular Ischemic Syndrome, can cause vague episodes of vision loss, pain and sometime small hemorrhages within the retina. These eyes can rapidly develop abnormal new vessel growth inside the eye and severe glaucoma after otherwise uneventful cataract surgery.
Is this damage permanent? Not everyone who suffers a blocked blood supply to the eye or brain has permanent damage. A temporary blockage of blood supply to the brain, called a transient ischemic attack (TIA), may result in muscle weakness in the face or an arm or leg, lasting only a few minutes to a few hours. A temporary blockage of blood supply to the eye, called amaurosis fugax, or fleeting blindness, can cause a temporary loss of vision in one eye. This sometimes appears as a dark curtain descending over all or part of the vision in that eye and may last for a few minutes to several hours. Both amaurosis fugax and transient ischemic attacks are possible warnings of a serious problem involving the blood supply to the eye or brain. They should be reported to your eye doctor or primary care physician.
Are There Other Signs of Carotid Artery Disease? As part of a routine eye exam, the eye doctor may dilate the pupil to examine the retina at the back of the eye. During this procedure conditions are sometimes discovered, which may indicate an increased risk of stroke. If a piece of cholesterol, or plaque, is found during a routine eye exam, further evaluation may be indicated. Other similar plaques may break off from the carotid artery, block the brain's blood supply and cause a stroke.
What Further Tests or Treatments May Be Needed? Rarely, an inflammatory condition called Giant Cell Arteritis can inflame smaller vessel supplying the eye or brain. This can be diagnosed with a blood test and/or small artery biopsy. Ultrasound can provide a very detailed look at the carotid flow. Sometimes, a special X-ray test called a carotid angiogram may be done. Angiography involves injecting an iodine-containing dye into the artery and taking pictures of the blood flowing into the brain. If an abnormality is found, surgery may be recommended to correct the blockage. With some obstructions, only medications are necessary.
Routine, comprehensive medical eye examination can help ensure healthy vision and can provide important information concerning carotid artery disease. If problems are detected, your eye doctor will work with your other medical doctors to coordinate your complete medical care.-
Retinal Detachment
How Does the Retina Become Detached? The eye is like a tiny camera, with lenses in the front and film in the back. The film is called the retina. It lines the back three quarters of the eye like an inner tube. The center of the eye is filled with a jelly-like material called vitreous. It is thick during childhood, but later becomes watery. In many cases, the back layer of the vitreous can pull away from the retina, and in some cases, tear it. Fluid can then leak through the tear and allow it to detach from the back of the eye. This causes loss of vision because the retina relies on the back wall of the eye for its nourishment.
What Are the Symptoms of Retinal Detachment? When the vitreous gel peels away from the back of the eye, the normally clear fibrous strands clump together and cast shadows, referred to as floaters. When the gel pulls or tears the retina, this stimulates the retina and may cause flashing lights to be seen. Flashes and floaters are the warning signs of a possible impending retinal detachment. Flashes and floaters do not always signify a retinal tear or detachment. Prompt evaluation by an eye doctor may find a retinal tear before it causes a retinal detachment. Laser surgery or cryotherapy (localized freezing treatment) may prevent the retina from detaching and save the patient from needing to have a more serious operation.
Treatment for Detached Retina There are several types of surgery that can repair a detached retina. The surgery usually consists of one or more of the following procedures:
Scleral Buckle A plastic band is often placed around the eye to indent and support the area of the tear. It may extend all the way around the eye, like a belt, or it may be fixed to only one area. The patient cannot see or feel the band once the eye has healed. The scleral buckle is meant to stay in place for your entire life. This procedure has a longer healing time and except in unusual cases is not used much any more.
Pneumatic Retinopexy If the tear causing the retinal detachment is in the top half of the eye, it may be possible to seal it with a gas bubble injected into the eye. This is combined with special head positioning to push the bubble against the tear, and laser or freezing to “glue” the tear back into position and prevent redetachment. This is a good treatment option for only occasional retinal detachments. Your surgeon will advise you on your individual case. If the bubble does not work, scleral buckling and/or vitrectomy may be recommended.
Vitrectomy In more complicated retinal detachments, vitrectomy surgery may be necessary. This operation removes the vitreous jelly as well as any scar tissue or blood, which may have accumulated. The vitreous
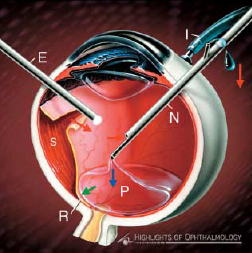
is replaced with special fluid or sometimes a gas bubble. The fluid or gas is replaced by the eye’s own fluid over time without any further surgery.
Before the Operation A general physical examination is part of the preoperative routine. In some cases, other laboratory testing is necessary, depending on your age and physical condition. We will consult with your primary care physician to discuss your case and secure clearance for your surgery. An anesthesiologist will interview you and assist your doctor with preoperative medications.
The Operating Room An intravenous line will be placed into an arm or hand vein. If you are having general anesthesia, you will not be aware of the operation. You will be in the recovery room when you wake up. If you are having local anesthesia, a tranquilizer will be injected in the intravenous line. You will be relaxed and sleepy. You may or may not fall asleep. A local anesthetic will be injected around, but not into your eye. You should feel no pain.
After the Operation Following surgery you will remain in the recovery room for a short period under special supervision. You will have a patch on your eye. Some pain is to be expected, which is controllable by oral or injected medication. Some nausea is not uncommon and will also be treated with medication. If vomiting should occur after surgery, this will not harm the eye. The intravenous line may be discontinued once you are fully awake. Most retinal surgery can be done as an outpatient, but rarely an overnight hospital stay is required.
Postoperative Examination and Advice You need to be examined the day after surgery and usually again within a week. At this time, you will be given an eye drop prescription, eye pads, tape and instructions. The main purpose of the eye patch is to soak up tears, and it may be removed once tearing has subsided. You may wash your hair at home or have it done at a hair salon. You should not allow running water directly on the operated eye, so you may want to wear an eye patch while showering and remove it when done. Most people may resume their normal lifestyle as quickly as they wish and return to work within one to two weeks following surgery. Your eye may feel scratchy or sore, and you may have a stuffy nose for a few days after surgery. You may do whatever is comfortable, but should rest as needed. If a gas bubble is placed in your eye during the surgical procedure, you should not fly in an airplane or receive anesthetic gases. Either can cause the bubble to expand, causing pain and possible damage to the eye. Your doctor can determine when it is safe to fly or have anesthetics. Your physician will tell you if special positioning or activity limitations are necessary.
Patients ultimately return to their referring doctor for their continuing care. If you wear glasses or contact lenses, the power of the lens may change as a result of your surgery. We usually do not recommend changing your glasses or contact lenses for about two months following surgery to allow the new prescription to stabilize.The Outlook If your vision was good before surgery, the chances are excellent that you will maintain normal or near normal vision following surgery. If the vision was poor before surgery, especially if the detachment was longstanding, the visual return may be slow and incomplete. A single operation successfully re-attaches the retina in more than 90 percent of cases. In a few cases, scar tissue may begin to form inside the eye, which pulls on the retina causing it to re-detach. If the retina should detach again, it usually does so within several months of surgery and can often be repaired with another operation. Great strides have been made in retinal detachment surgery over the past 20 years. Retinal detachment, which was once an incurable problem, can now be helped in the vast majority of cases.
-
Lattice Degeneration
Lattice degeneration is thinning and weakening of the retina, the light-sensitive layer of cells lining the back of the eye, that can lead to a retinal tear.
The vitreous, a clear gel-like substance that fills the inside of the eye, is contained in a sac loosely attached to the retina. As one ages, the vitreous takes on a more fluid consistency and the sac sometimes separates from the retina. In lattice degeneration, there are places where the sac is strongly attached to the retina and pulls on it. This pulling weakens the retina and creates lattice lesions that look like white crisscrossing lines on the retina.
If part of the vitreous sac becomes detached from the retina, the friction and pulling where it is still attached can create a tear in the retina. Lattice degeneration can sometimes cause retinal detachments when holes or tears in the lattice formation permit vitreous fluid to get under the retina.
Fortunately, most people with lattice degeneration do not develop a retinal detachment. Preventive treatment of lattice degeneration has not been shown to prevent retinal detachment, but lattice degeneration should be monitored. If you have a history of lattice degeneration, you should be aware of the symptoms of retinal tears and detachment.-
Retinopathy of Prematurity
Risk Factors and Monitoring
Most premature children do not develop ROP, but when it does occur, the result can be very serious, and so it is vitally important to monitor at risk patients and offer treatment in a timely manner. The most important risk factor is prematurity itself. Small birth weight and not oxygen use, is the only strongly associated risk factor. Oxygen's main role is probably that it allows very small children to live, and a percentage of these children develop ROP. Other lesser risk factors include the other illness encountered by premature children. We use specific and very cautious criteria guiding ROP monitoring. This is designed to catch all at risk children and to ensure timely laser or other treatment if it becomes necessary.
By the "due date", most children either develop ROP needing treatment, or they mature to the point that close monitoring is no longer necessary. If your child leaves the NICU before reaching retinal maturity, it is extremely important to keep follow up visits as an outpatient. We make extreme efforts to facilitate this followup, but we cannot control all events and cannot be responsible if you fail to keep these critically important visits. Even with retinal maturation, premature children are at a somewhat increased risk of developing near-sightedness or strabismus (crossed eyes). For this reason, an additional screening exam is recommended at about one year of age.
Progression of Disease and Treatment
Children who develop Stage 3 ROP, with the development of abnormal new blood vessels over the retina are very likely to need retinal laser surgery. This is real surgery and not to be taken lightly, but it is done in the nursery, and is not terribly stressful to the child. It is done with topical anesthesia and close monitoring by the NICU staff. In many of these children, one or more laser treatments is successful in reversing the vessel growth and preventing progression to the more severe stages of ROP.
In some cases, the disease progesses in spite of laser treatment, with the development of traction and retinal detachment. Without further treatment, this is usually visually devastating, allowing little or no useful vision in affected eyes. This result can sometimes be avoided with surgery called vitrectomy. Vitrectomy is complex surgery to remove the gel from the back chamber of the eye along with any scar tissue or blood, in an attempt to relieve traction and detachment of the retina. Every attempt is made to avoid removing the eye's natural lens, because this lens is very important for focusing and visual development. Sometimes the lens must be removed and must later be replaced with a contact lens or, eventually, surgical lens implantation.
Obviously, more serious disease is more visually threatening. When ROP worsens, it is virtually always in spite of treatments already applied in an attempt to stop it. We watch patient's extremely closely an offer treatment at the earliest recommended times. We also work very closely with the ROP specialists at William Beaumont Hospital in Detroit, considered to be one of the top ROP research centers in the world. We will discuss any details that are applicable to your child's individual circumstances.-
Vitrectomy Surgery
Things to Know Before, During, and After Retinal Surgery
Level of Urgency
Different types of retinal surgery have different levels of urgency. The most urgent cases involve infections inside the eye and traumatic ruptures or lacerations. These are true emergencies and need to be treated immediately. Retinal detachments are not usually true emergencies but they are urgent, and require treatment usually within a few days. Longstanding detachments can be treated on an elective basis. Some retinal problems, such as macular holes and macular puckers are non emergent and can be treated at any time on an elective basis. We will discuss the degree of urgency of your problem with you individually.
Medical Clearance
Whether the case is urgent or not, we do need to make sure that your surgery is as safe as possible. At a minimum, this entails a careful review of your medical history and discussion with the anesthesia team. We also obtain appropriate medical clearance from your medical doctors. Depending on the type of anesthesia used, we may need to obtain an EKG and certain blood tests. Sometimes a chest x-ray is necessary, especially if you are over 50 or have lung ailments.
About Your Medicines
If you are taking blood thinners, we may ask you not to take such medicines for a few days prior to surgery. If the surgery cannot wait, or if your doctors do not want you to withhold your blood thinners, we can take measures to accommodate your situation. You can take your normal medicines as usual up to the day of surgery. On the day of surgery, you should skip nonessential medicines, but go ahead and take any medicines for your heart or blood pressure on schedule with a small sip of water. You are not to eat or drink ANYTHING else after midnight of the night before surgery, and if you are diabetic you should skip any oral diabetes medicines and take no more than half of your normal insulin. We may ask you to skip it altogether. If you take glucophage, you should stop it two (2) days before surgery if possible.
The Day Before Surgery
You may eat normally and follow yor normal routine on the day before surgery, but DO NOT drink any alcoholic beverages. Also, if at all possible, do not smoke or use any tobacco products or recreational drugs. Relax and get a good night's sleep. You should not eat or drink ANYTHING after midnight. (Not even coffee, tea, or water, and especially not juice.) See the section above regarding your medicines. Before bed, wash your face with an antibacterial soap.
The Day of Surgery
Devote the day to surgery. This is not a day that you should plan anything else. You need to arrive at the surgery center at least an hour, and preferably an hour and a half before your surgery. Do not wear ANY eye makeup on the day of surgery. You may shower and brush your teeth normally, but do not drink anything. After you return home from surgery, do not plan on doing anything or going anywhere. You should, at the very least, take it easy, and we may ask you to maintain a special head position. Some types of retinal surgery cause significant discomfort for the first day and others only mild scratchy discomfort. You will feel better if you keep still and do nothing that might raise your blood pressure. In most cases, simple over the counter Tylenol or Advil are all that is necessary for comfort. If we anticipate more than the usual discomfort, we will prescribe an analgesic.
After Surgery
The First Postop Day
We need to see you the day after surgery. You will have a patch on after surgery, which in most cases, we leave on until the first postop day check. In most cases, we leave the patch off after that. We will check your eye and start you on one or more eyedrops. We will also give you wrap-around sunglasses that will fit over most regular glasses to help you keep out the sun and wind and will protect your eye. In most cases, the vision in your operated eye will still be blurry, possibly even worse than preoperatively. This is because the eye will be red and teary, because we sometimes use medicines that blur the vision, and of course because your retina needs to heal.
Driving and Other Activities
Because the vision is blurry, your depth vision is also affected, so you should not drive or operate hazardous machinery until well after surgery. How long depends on your vision and what you want to do. We will discuss your limitations with you individually. In some cases we may inject air or special gas mixtures into the back chamber of the eye. This is usually to hold the retina still and help it to stabilize or heal better. While you have a bubble in your eye, it is EXTREMELY IMPORTANT that you not get into an airplane or have certain types of anesthetic gases. Either could cause the pressure in the eye to rise drastically, which is very painful and can be very dangerous to the eye. If you have a bubble in your eye, we will have you wear a medical alert bracelet until it is gone. The bubble will dissolve on its own in a few days to a few weeks.
Your Eye Comfort
In most cases, the eye is fairly comfortable after taking the patch off, but after some surgeries it may be uncomfortable for several days. Sometimes, the eye pressure is high or low following surgery, either of which can cause pain. We will watch this and other factors very closely.
Positioning
In some cases, we may ask you to keep your head tilted or face down for a few days or even longer. This is VERY importatnt to the success of your operation, so please do your best to follow these instructions very carefully.
What the Future Holds
What the future holds depends entirely on the nature of your eye problem. We will discuss your individual circumstances with you directly. Retinal surgery has undergone major advances in recent years, and new techniques and refinements continue to appear. There are still many serious problems for which we have no good solution, but in most cases, there is good cause for optimism. We will work with you to give you the best possible outcome, and if you ever have any questions or problems, you should discuss them with us right away.-
Retinal Dystrophies and Retinitis Pigmentosa
Separating Facts from Fear
Being diagnosed with Retinitis Pigmentosa can be very frightening, not only because it is a serious
condition, but also because there is so much old and incorrect information associated with the diagnosis. Before you reach too many conclusions, wait. It will be much less scary if we take a few minutes to separate fact from fiction. It is very important to know not only what the diagnosis means, but also what it does not mean. For instance, it does not mean that you are going to lose your vision soon. Not this year, and probably not even in the next 10 years. It is true that there are not many treatments at this time, but this may not be the case in the future, during the time that you still have saveable, treatable vision. It is also possible to adapt quite well to your limitations with help from people who know the problems, and have perhaps dealt with them personally. So, let's go over some basic information. The following is a brief review. Additional information, and resources are available from the links on the left.
What is RP?-
Retinitis Pigmentosa is a large group of inherited diseases, called "retinal dystrophies", causing retinal malfunction and gradual loss of vision. There are many different forms, but all cause a gradual decline of vision, which eventually over years results in severe or even total vision loss. Most types of RP result first in decreased night vision and peripheral (side) vision. Only a few types cause early loss of central vision. Progression is usually extremely slow with changes noted over years or even decades. Rapid vision loss over weeks or months is extremely rare.
The many subtypes of retinal dystrophy-
A "dystrophy" is a disease caused by an abnormality in a gene, causing some part of the body to malfunction. There are many genes controlling the function of the retina, so a retinal dystrophy is a gene abnormality resulting in retinal malfunction. There are dozens genes controlling the retina, and there are dozens of different types of retinal dystrophy, all with very long and strange sounding names. For simplicity, they are collectively referred to as Retinitis Pigmentosa, or "RP". Some cause malfunction of the "rods", retinal light receiving cells that control most of our night vision and side vision. RP affecting these genes are call "rod" or "rod-cone" dystrophies, whose first symptoms are problems with the night and side vision. This is sometimes called "night blindness". Other dystrophies cause malfunction of the "cone" light receptors, which control the central, color, and daytime vision. "Cone" dystrophies result in earlier loss of central vision, color vision, and sometimes light sensitivity or "day blindness".
RP is usually an inherited disease-
RP is usually an inherited disease, meaning that the abnormal gene is passed along in a family from generation to generation. Each of us has two copies of every "autosomal" gene, one from our mother and one from our father. If the abnormal gene is "dominant", then it only takes one abnormal copy to cause the disease symptoms. If you "do the math", it turns out that dominant RP shows up in about 1/2 of an affected person's children. Occasionally, RP appears "out of the blue", with no previous family history. Like dominant inherited RP, this is usually the result of one abnormal gene copy, and it is usually passed one from the first affected person in a dominant pattern.
If the abnormal gene is "recessive", it means that you need two copies with the same abnormality to have the disease symptoms, one bad copy from each of your parents. These cases are very rare. If you have recessive RP, and your spouse does not, then each of your kids will have one abnormal gene, from you, and in all liklihood one normal gene from your spouse. Your kids will "carry" the gene but will not have the disease. Unless they marry a blood relative, it is very unlikely that they will pass the disease on to their children, although about half of there children may carry the gene. Two carrier parents are at risk of having one fourth of their children affected and one half of their kids carriers.
There is one other main inheritance pattern, called "X linked recessive". Some genes are carried in the female "X" chromosome. This means that males have only one copy of that gene, from their mother. Women have two copies, one from mom, and dad gives them his only copy. If mom has an abnormal "X" gene, she may pass it along to half of her sons (it is almost certain that her other copy is normal), and they would have the disease symptoms. Half of her daughters will be carriers, like her. As you can see, the inheritance questions get very complex, and you should talk in detail with your doctors about the inheritnace questions that may apply to your situation.
Could it be something besides RP?
Yes. There are many other gene abnormalities that affect vision, and there are infections and inflammatory diseases that can mimick RP. Such inflammatory diseases inlude congenital rubella (German Measles), syphilus, tuberculosis, various viral diseases, and even some rheumatoid diseases. Other gene abnormalities include "X-linked retinoschisis", which causes retinal detachment and macular (central vision) malfunction. There is a group of diseases called "congenital stationary night blindness", which as the name suggests causes night blindness but does not progress much over time. Juvenile Macular Degeneration, Stargardt's Disease, Fundus Flavimaculatus, and Pattern Macular Dystrophy are some of the many names you may hear as you learn more about RP. These are all important but very different diseases that need to be considered as we deal with your individual circumstance. Your diagnosis can usually be very precisely determined by the specialized testing that is now available.
What tests are used to diagnose RP?
RP itself is a group of diseases that all cause some abnormality of the electrical transmission of vision in the photoreceptor cells in the retina. Other diseases cause transmission abnormalities of other types or in other locations in the retina. The type and location of electrical malfunction can be detected using tests that measure electrical activity. This is called electrodiagnostic testing. The main types are "Electroretinography" or ERG, "Electro-Oculography" or EOG, and occasionally "Visual Evoked Response" or VER. These are very delicate tests to do, requiring a very specialized lab set up, but except for involving bright lights, they are not unpleasant for the patient. In order to obtain the best quality testing, we often send patients to an academic center where this testing is done frequently. The Berman-Gund Laboratory at Massachusetts General Hospital has new ERG technology that can help provide detailed information capable of predicting, within a few years, how many years of useful vision a patient may expect. This information can be invaluable, not only to allay the fear of the unknown, but also to help in life and career planning. Other tests include visual field testing to measure side vision and various photographic tests, all of which are done here in our offices. Electrodiagnostic tests are done initially at the time of diagnosis, but do not usually need to be repeated very often. Other tests are done to follow functional performance, such as to evaluate a patient for driving or specific job tasks, or to evaluate common problems that sometimes arise in RP patients, such as cataracts, glaucoma, or macular edema.
Other conditions may be more common in RP patients-
While treatment of the RP itself is currently limited to vitamin therapy, certain other very treatable conditions are more common in people with RP. Certain types of cataracts occur sooner and may progress more quickly in patients with RP. When necessary, this is easily treated with cataract surgery. RP patients may also develop swelling (edema) in the macula, the reading portion of the retina. This can be treated with eyedrops or pills to decrease inflammation. Glaucoma may be more common, and certainly can progress more rapidly in RP patients, and this is treated with drops, laser, or surgery. Because of these issues, it is very important for RP patients to have regular eye checkups.
What about current RP treatment?
Currently, the mainstay of RP treatment is limited to dietary supplementation with Vitamin A palmitate. This is a DIFFERENT form of Vitamin A than the beta-Carotene or regular Vitamin A found at the local pharmacy. These common forms are WORTHLESS in RP treatment. Some years ago, a large multi-center study found that extra Vitamin A in the highly soluble palmitate form increased electrical activity in the retina by several microvolts. In many patients this may be enough to add several years of useful vision in the patient's life. The same study found that supplemental vitamin E not only didn't help, but may actually be detrimental. The learning point here is not just to avoid high dose Vitamin E, but to be very careful about chasing every new dietary fad without waiting for experimental support. Vitamin A Palmitate is not ea-sy to find, but it can be easily obtained from Akorn Pharmaceuticals (800-932-5676). Ask for "Palmitate-A 15000". You should take 15000 units per day. Less is less effective and more can be toxic.
Other treatments will likely be available in the future-
RP in most forms progresses very slowly. During the lifetime of a patient diagnosed with RP today, it is very likely that new and meaningful treatments for RP will appear. Even now, there are several avenues of treatment research. New nutritional studies are currently underway. Gene research is very complex, but animal experiments have yielded astonishing early results. There are also ongoing studies into artificial retinal stimulation and even bypassing the retina altogether using video technology to stimulate the visual areas in the brain. We will keep you informed about these things at your visits and through this website.-
Uncommon Retinal Diseases
Birdshot Retinochoroidopathy (BR) Birdshot retinochoroidopathy (BR) is a rare, inflammatory condition of the retina and choroid, the layer of blood vessels under the retina. BR usually occurs in Caucasian women over the age of forty.
The cause of BR is unknown. It usually affects both eyes. Symptoms are poor vision, night blindness, and disturbance of color vision. Pain is rare.
Fluorescein angiography, a test for evaluating the retina and choroid, detects BR's characteristic cream-colored spots, similar in appearance to the splattered pattern of birdshot from a shotgun.
BR is a chronic disease that flares up and then goes into remission. Although some people eventually lose vision, others maintain or recover good vision.
If you have been diagnosed with birdshot retinochoroidopathy, it is important to see your ophthalmologist regularly.
Coats' Disease Coats' disease is a chronic, progressive disorder that affects the retina, the light-sensitive nerve layer at the back of the eye. Coats' disease is an abnormal growth spurt of the small blood vessels (capillaries) that nourish the retina. The fragile abnormal vessels break and leak the clear serum part of the blood into the retina, causing the retina to swell.
Coats' disease usually affects children (especially boys) in the first ten years of life, but it can also affect young adults. The condition affects central vision, typically in only one eye. Severity can range from mild vision loss to total retinal detachment and blindness. No cause has yet been identified for Coats' disease.
The leaking blood vessels can be treated with laser surgery or cryotherapy (freezing). If the retina is detached, a vitrectomy to replace the vitreous (the clear gel-like substance inside the eye) with a gas bubble may be necessary to restore vision
Macular Dystrophy Macular dystrophy is a hereditary condition in which the macula degenerates. The macula is the part of your retina responsible for acute central vision: the vision one uses to read, watch television, and recognize faces.
Symptoms of macular dystrophy can range from minimal vision loss and disturbance of color vision to profound loss of reading and night vision. The most common types of macular dystrophies, which tend to appear early in life, are Best's disease, Staargardt's macular dystrophy, and bull's eye maculopathy.
Considerable research is directed toward finding the hereditary cause of many types of macular dystrophies. With further research it may be possible to develop medical treatments to prevent or slow the progression of macular dystrophy.
Low-vision devices can help affected individuals continue with many of the activities of daily life.
Stargardt's Disease Stargardt's is an inherited disease that affects the retina, the layer of light-sensitive cells lining the back of the eye. It usually becomes apparent between the ages of 8 and 14. Boys and girls are equally susceptible and more than one child in a family may have it.
Stargardt's disease begins with slightly blurry vision that gradually gets worse. By the late 20s, vision is typically about 20/200, the level labeled legally blind. Remaining vision is good enough for most people to live fairly normal lives, though they won't drive, or read without using magnification devices.
A build-up of lipofuscin (fatty substance) in retinal cells is thought to cause Stargardt's disease. The buildup typically happens in the central retina, or macula, where it resembles beaten bronze. Or, it can occur in the side retina where it causes small white flecks. This form is called fundus flavimaculatus. Angiography, a special photograph of the retina, may aid in the diagnosis. Although no specific medical or surgical treatment is available, glasses and magnification help affected people adapt to the disease.
Retinoschisis Retinoschisis is a genetic eye disease that splits the retina, the light-sensitive layer of cells lining the back of the eye. It occurs in two forms, one affecting young children, the other older adults. Both forms usually affect both eyes, though one eye may be worse than the other.
Because the disease is inherited on the X chromosome, childhood retinoschisis occurs in boys more than girls. It is usually detected because of poor vision.
If the split retina involves the peripheral or side retina, peripheral vision is lost. One is also at risk for a retinal detachment. But more commonly, retinoschisis affects the macula, the area of the retina responsible for central vision. In this location, one loses central vision.
Peripheral retinoschisis, more common in adults, is usually caused by aging and does not affect vision, but it can cause a retinal detachment. If detected early, a retinal detachment can be treated with surgery or laser therapy.
